Ob/Gyn #
OCPs 101 #
NO changes for 3 months Takes body a little bit to get used to everything => can start chasing your tail if making too many changes too quick
- Start at 20mcg estrogen
- If PMS-like symptoms => ↓ estrogen
- If spotting => ↑ estrogen
- Usually start w/ levonorgestrel
- If acne/bloating => switch progesterone from levo to norethindrone
- If you decrease estrogen, generally decrease progesterone too
- If pt “too moody” => try nuvaring
- Depoprovera gotchas
- Long return to fertility
- Weight gain
- If pt with pre-existing acne => Yaz (drospirenone + estrogen)
- Mirena
- Not fun being placed, but tolerable
- More progesterone
- More chance amenorrhea
- More chance of acne
- More moodiness
- Kyleena
- Less progesterone
- Less moodiness
- Less acne
- Less chance of no period
- Less progesterone
- Cheap OCPs
- Lutera (20) ← default to this, sliightly lower estrogen
- Sprintec (35)
Ovarian Cysts #
- Simple cyst is physiologic
- Repeat US in 6 weeks to confirm it’s simple
- Treatment
- OCPs
- If on OCPs
- Journal symptoms
- APAP/ibuprofen/naproxen before the day to control
Trimesters #
- 1st: 0-14wks
- 2nd: 14-26wks
- 3rd: 27-40wks
OB Visits #
| Gest. Age (wks) | Exam | Labs | Other |
|---|---|---|---|
| 8 | US, preg confirmation | Genetic questionaire, famhx, med problems | |
| 12 | Full exam, breast, pelvic | CBC, TSH, HIV, RPR, GC/CT, HepB sAb, Rub, cell free DNA, Nuchal transulcency (if doing sequential), Urine cx | PAP if not UTD |
| 16 | FHT, fundal height | AFP (Cell free DNA) or Quad | |
| 20 | FHT, fundal height | Anatomy Scan | |
| 24 | FHT, fundal height | Glucola instructions | |
| 28 | FHT, fundal height | Rhogam, 1 hr Glucola test, antibody screen, CBC, 1hr gluc tolerance test | |
| 32 | FHT, fundal height | Tdap | |
| 34 | FHT, fundal height | ||
| 36 | FHT, fundal height | GBS | |
| 37 | Cervical exam, FHT | ||
| 38 | Cervical exam, FHT | ||
| 39 | Cervical exam, FHT | ||
| 40 | Cervical exam, FHT | ||
| 41 | Cervical exam | NST, AFI | Schedule induction |
AFI #
- Sum of deepest pocket of amniotic fluid in each of four quadrants (Radiopedia)
- Must keep probe perpendicular to floor (i.e. straight up and down)
- Normal 5-25cm
- <5cm OR single deepest pocket less than 2cm = oligo
Thyroid #
Titrate to TSH of 2.5 or below for pregnant or trying to get pregnant patients.
Anemia in pregnancy #
- Definition: <5%-ile
- 1st tri 11g/dL or 33%
- 2nd tri 10.5 or 32%
- 3rd tri 11 or 33%
- Plasma volume ↑ 40-50%, erythrocytes only ↑ 15-25%
- Prevalance ≈2%
- Black women: ≈3.5%
- White women: ≈1.8%
- Per trimester
- 6.9%
- 14.3%
- 29.5%
- Increases risk of:
- Low birth weight
- preterm delivery
- perinatal mortality
- PPD?
Mechanism #
- Production ↓
- Lack of materials
- iron
- B12
- Folate
- Broken machienery
- bone marrow issues/supression
- hypothyroidism
- renal dysfunction (EPO)
- bone marrow issues/supression
- Lack of materials
- Destruction ↑
- Inheritied
- sickles, thalassemias, hereditary spherocytosis
- Acquired
- Autoimmune
- TTP
- HUS
- Malaria
- Inheritied
- Broken cells
- Thalessemias
- Hemolytic anemias
- Loss
Screening #
- CBC at intake and at 24-28 weeks
Iron supplimentaiton #
- need 27mg Fe per day
- Start all women on low dose (CDC+, ACOG+, USPSTF +/-)
- Consider IV iron if severe or if can’t tolerate oral iron
- transfuse
- Hgb <6g/dL => affects baby
- Consider cell salvage
- Jehovah’s witness
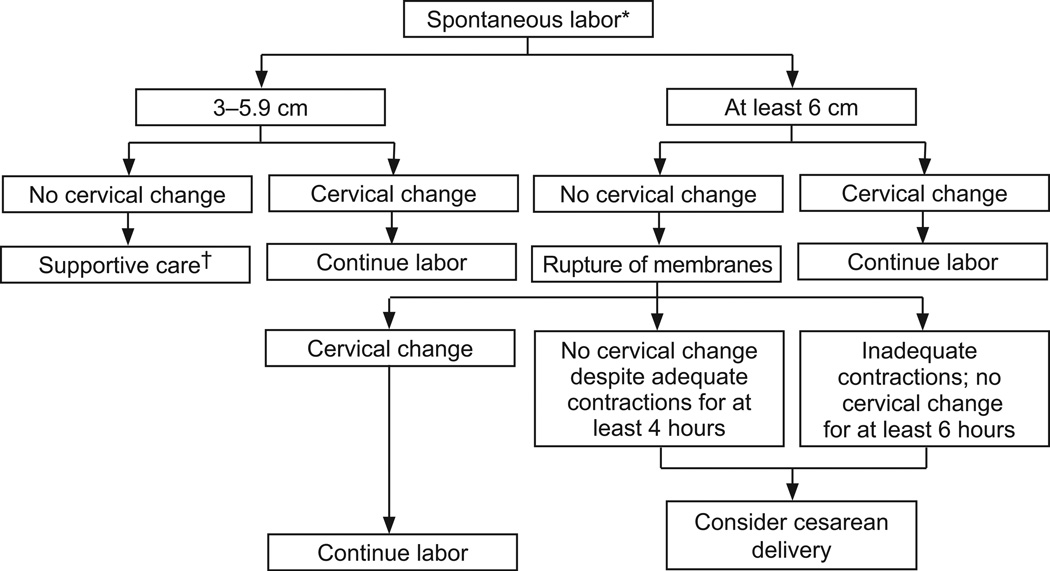
Labor #
Real labor contractions happen every five mins, lasting one minute
Labor = cervical change + contractions
Anticipated amount of time for active labor:
- G0 w/ epidural 4hrs
- G0 w/o epidural 3hrs
- G1+ w/ epidural 2hrs
- G1+ w/o epidural 1hr
Progression #
Pain Control #
Four options:
- Au Natural
- Nitrous oxide
- Relaxes you, but doesn’t really treat pain
- IV fentanyl
- Doesn’t take away all the pain, but works and goes fast
- Great for CRB placement
- Can’t give close to delivery as makes sleepy babies
- Epidural
- Can’t walk
- Slows second stage of labor by approx. 30 mins (not a huge deal)
Morphine sleep #
- morphine
- phenergan
- recheck in 8 hours, can go home after that
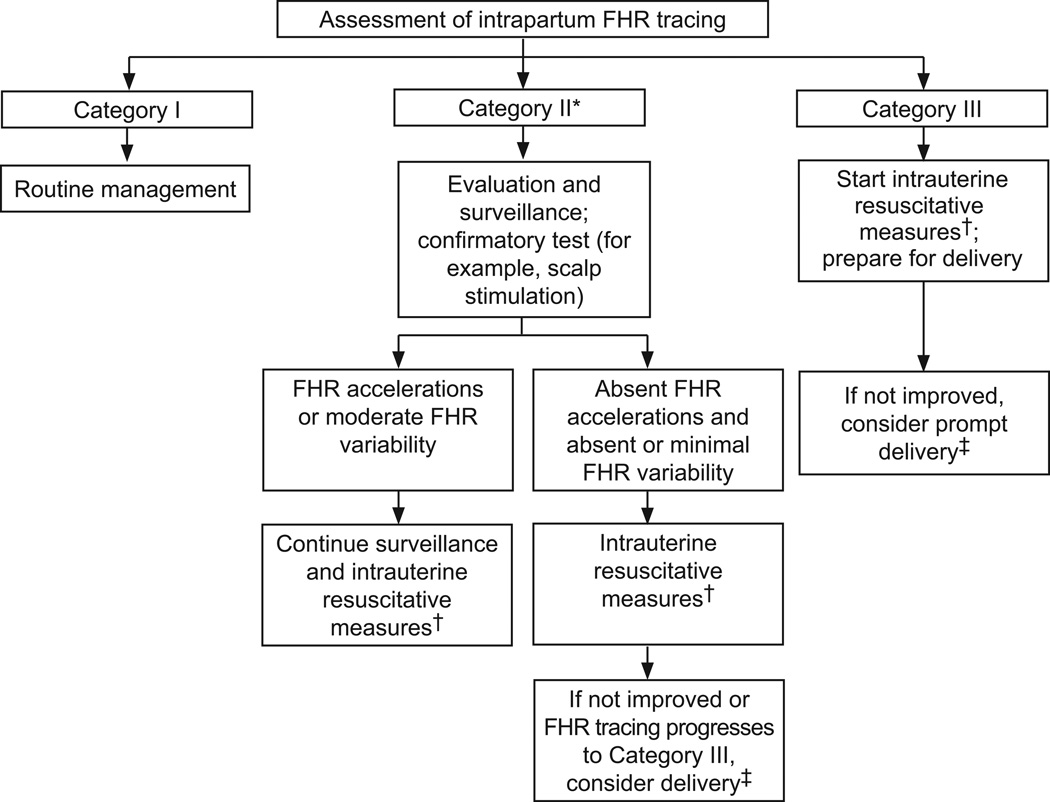
Strips #
VEAL CHOP
| Signal | Event |
|---|---|
| Variable | Cord compression |
| Early | Head compression |
| Accels | Ok! |
| Lates | Prolapse (cord) |
Examples and practice
Inductions #
- Cytotec plus foley
- Pitosin then AROM
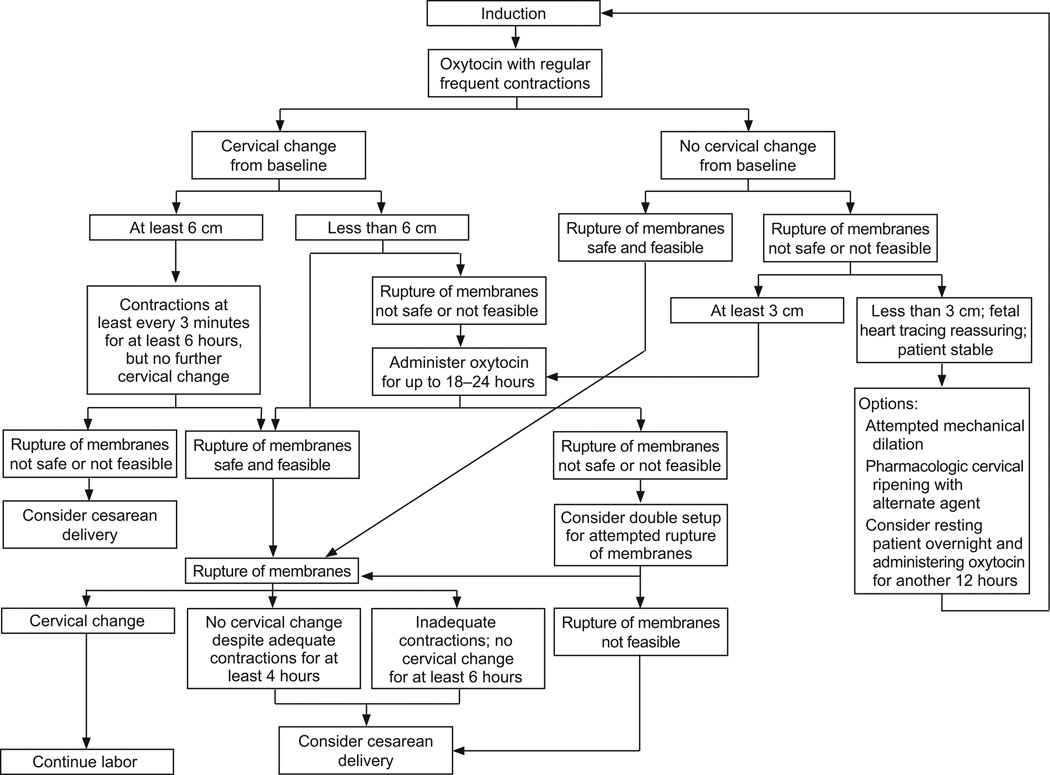
Failure #
- No change in 4hrs with adequate contractions
- No change in 6hrs regardless of contractions
Cervical Change #
- Cytotec
- PO or vaginal q4hrs
- Cervadil
- vaginal q12hrs
- Foley
- 50cc; dilates to 3-4cm
- Cook cath
- 50cc; dilates to 5cm
- Walking (natural)
- gravity
- Nipple stim (natural)
- Stim one nipple for a 30 sec contraction
- Switch nipples
- Sex (natural)
- oxytocin from orgasm
- Strip membranes
- thought to release endogenous prostaglandins
Check Bishop score
Contractions #
- AROM
- Best in multips who want to go “natural”
- Pitocin (oxytocin)
- Start at 2
- Increase by 2 every 30 mins
Post Partum Hemorrhage (PPH) #
>1000mL within 24hrs of delivery (either vaginal or c/s)
Treatment #
- Pitocin
- Can give two bags
- Misoprostol (Cytotec) 800-1000mcg rectally
- Can give 200mg PO
- Slow onset
- Can cause N/V, mild fever
- Methergine 0.2mg IM q2-4hrs
- Fast acting
- Contraindicated in patients with hypertension (relative)
- 6 dose max
- Some use the 2-4-6 rule
- 0.2 every 4 hrs for 6 doses
- Some use the 2-4-6 rule
- Hemabate 0.25mg q15-90 minutes
- Contraindicated in patients with asthma
- 8 dose max
- Causes wicked diarrhea
- Give with lomotil or nurses will hate you
- TXA 1-2g per 500mL-1L bag
- Can repeat 1x
- Only helps with clotting, not a uterotonic
Hypertensive Diseases of Pregnancy Spectrum #
| Condition | Dx | Tx | Delivery |
|---|---|---|---|
| cHTN | >140/90(a), <20wks | None, baseline PIH(b) labs prenatally | No meds: 38w0d - 39w6dMeds controlled: 37w0d-39w6dMeds uncontrolled: 36w0d-37w6d |
| gHTN | >140/90(a), >20wks, wnl p/c | 37w0d | |
| PreE w/o SF | >140/90(a), >20wks, p/c >e; 0.3 | 37w0d, PP enoxaparin? | |
| PreE w/ SF | >160/110 for q15min repeats or two >4 hrs apart | Mild range + lab abnormalities(c)Mild range + intractable HA or vision changes (spots, floaters, not usually blurry)Pulm edema (CXR) | Mag |
| HELLP | Hemolysis (LDH >600)LFTs 2x upper limitLow platelets (<100k)(must have all of the above) | Mag | Immediate delivery |
a. Either, 4 hours apart
b. PIH labs: CBC (plts), CMP (Scr and LFTs), P/C, UA, LDH
c. One of: plts <100k, LDH >600, Scr > 1.1 or 2x baseline, LFTs 2x upper range of normal
Pre-eclampsia (PreE) #
Treatment #
Magnesium (Mg)
- Bolus 4-6g
- Can give 5g IM x2 (both cheeks)
- Infusion 2g/hr
- Reflexes disappear as becomes therapeutic (pts are hyperreflexic when in PreE)
- UOP needs to be 0.5mL/kg/hr
- Mg renally excreted
- Reversal agent: Ca gluconate
- Only really used if cardiac toxicity
- Toxicity:
- >15 respiratory paralysis
- >25 cardiac abnormalities
Miscarriage #
Criteria:
- No cardiac activity after US with cardiac activity
Management #
- Expectant
- Misoprostol
- Only up to estimated 9w0d GA
- Higher risk of bleed and not completing past this GA
- 800mcg vaginally at bedtime
- Can take roughly 6 hours to start working
- 800mg ibuprofen at same time to help with cramping/pain
- Repeat x1 in 24 hours
- Only up to estimated 9w0d GA
- D&C
- Indicated if past 9w0d
Quick Ob Triage #
HPI #
- Vaginal bleeding
- Loss of fluid
- Contractions
- Complications of pregnancy
- Fetal movement
- Vitals
- FHTs/strip interpretation
- Rh +/- status
- GBS status
Labor Check #
- <34 Weeks
- Put baby on monitor
- If not contracting → discharge
- Check cervix
- if <5 and contracting → hold, recheck in few hours
- if >5 and contracting → admit
- Put baby on monitor
- >34 Weeks
- SSE collect FFN, KOH/wet mount (FFN no good if has had sex in last 24hrs)
- Transvaginal US for cervical length
- If >2.5cm → stable
- If 1.5-2.5cm → send FFN
- If <1.5 → corticosteroids/tocolytics
- Cervical exam
- If <2cm → stable
- If >2cm → corticosteroids/tocolytics
ROM #
- >34 Weeks
- Speculum exam (pooling, nitrazine, ferning/Amnisure)
- If positive, admit and check cervix
- If negative, check AFI
- Speculum exam (pooling, nitrazine, ferning/Amnisure)
- <34 Weeks
- Speculum exam
- Pooling, nitrazine, ferning/Amnisure
- KOH/wet mount
- Urine dip
- TVUS → cervical length
- If +ROM
- Admit
- Give latency abx
- GBS culture
- Mg if <32 weeks
- +/- MFM consult
- If neg ROM
- Check AFI
- Speculum exam
Gestational HTN/Preeclampsia (Pre-E) #
Pre-E = HTN + proteinuria after 20 weeks
- Monitor BPs
- Check sx
- Persistent HA (does not respond to acetominophen)
- Visual changes (scotoma; floaters)
- Epigastric pain
- DTRs
- Labs
- CBC (look for plts <100k)
- CMP (LFTs 2x normal, creatine > 1.1, Uric acid increased)
- UA (protein)
- Urine protein/creatine ratio (>0.3mg)
2nd/3rd Trimester Bleeding #
- Speculum exam
- CBC
- Coags
- Blood type (thinking Rhogam)
- Transabdominal US
- Placentation
- Signs of abruption
Trauma #
- Monitor for 4hrs
- Labs
- CBC
- Coags
- Type and screen (Rhogam)
- Transabdominal US
- Placentation
- Signs of abruption
- Consider Rhogam if abruption suspected
- Normal ACLS/Intubation
- Place pillow under R hip to help displace gravid uterus from decending aorta
Decreased Fetal Movement #
- NST
- AFI
Breastfeeding #
- Milk generally comes in between days 3-5
- Ok to have tender nipples for the first week, never ok after that
General info/fun facts:
- “Baby friendly” is a global designation steming from the WHO and UNICEF
- #1 cause of infant death worldwide is diarrheal illness from unclear water (i.e. used to mix formula)
- “Babies are like a drunk at a bar–they don’t care if it’s a bottle or a nipple…” -Carolyn (Lactation)
What to look for:
- Latch score <7 needs work
- Amount of time doesn’t matter
- Try to finish one side before switching → more fat at end
Breast infection with Serratia creates flourescent pink milk
To abruptly stop milk production:
- Cabbage leave
- Break veins
- Put in bra
- Replace when wilted
Engorgement #
- Actually an imflammatory process (not excess milk/too much volume)
- generally lasts 24-36hrs
- Ice, NSAIDs/anti-inflammatories
WIC #
- Doesn’t “favor”/push formula
- Will provide breast pumps and parts
- Will do both breast and formula but needs indication
Drug safety databases:
- LactMed (More libral)
- InfantRisk (more conservative but favored by lactation)
- Hale’s Medications and Mother’s Milk (book)
Pearls #
- Left hydronephrosis normal in pregnancy
- Normal physiologic changes in pregnancy: ↑ V_t, ↑ HR, ↓ BP
- Uterine inversion can cause a vaso-vagal response: ↓ HR, ↓ BP
- Limit caffiene to <200mg caffiene/day while pregnant (per ACOG, although so evidence that up to 400mg ok)
- Do a good vulvar/shallow vaginal exam on labor admits if have hx of HSV
- Breakthrough bleeding
- progesterone 200mg qday until stopped (Agestin is more expensive)
- OCP taper (for younger): 2 pills x 3 days then finish pack