Endocrine #
Hypogonadism (low testosterone) in Males #
Diagnosis #
Symptoms #
- Low libido
- Decreased morning erections
- Loss of body hair
- Low bone mineral density
- low impact fracture
- Gynecomastia
- Small testes
- infertility
- Less specific:
- Fatigue
- depression
- anemia
- reduced muscle strength/increased fat
Labs #
- ≥2 low AM (0800-1000hrs) total testosterone levels (must be with with symptoms as above)
- free testosterone only needed if you think sex-hormone binding globulin (SHBG) deficiency (older men)
- Elevated FSH and LH → primary hypogonadism
- Normal/low FSH and LH → secondary hypogonadism
- Consider
- prolactin → hyperprolactinemia
- Fe sat → hemochromatosis
- pituitary function test (likely referral to endo)
- MRI sella turcica
- Consider
Endocrine society strongly recommends against treatment unless diagnosis established as above, very hard to stop because of hypogonadism during recovery of pituitary-testicular axis
- Testosterone therapy eventually causes
- Small testicles
- Spermatogenesis supression
- Will contribute to BPH
- Increased CV risk
- Higher with injections, lower with gels/transdermals
Contraindications #
- Prostate cancer
- Erythrocytosis (Hct > 50)
- Severe OSA
- CHF (testosterone retains some sodium)
Monitoring #
- Initially every 2-3 months, when stable every 6-12 months
- Measure in between dosing days (i.e. if dosed on Mon, measure on Thurs or Fri)
- Gel has variable absorption, need two measurements to
- Hct < 50% (or above Hgb above upper limit)
- above normal should stop/lower therapy until normalizes
- If can’t keep Hct normal and total testosterone normal
- Eval for OSA/hypoxia
- If no treatable cause → phlebotomy
- Total testosterone 500-600 ng/dL
- Reduce if higher
- LH should normalize if adequately treated (will be high in hypogonadism)
- If fx at time of diagnosis or density in osetoporotic range
- DXA every 2 years until normalizes
DM1 #
Inpatient #
Common Scenarios #
- On basal-bolus
- If eating: continue home dosing (consider 20% reduction to be safe)
- If NPO: continue basal only
- On pump
- Verify settings
- Make sure pt has enough supplies while admitted
- Continue pump
- If no, convert to basal/bolus
DKA #
Converting insulin drip to basal rate #
Once gap closed and bicarb normalized:
- Add up total insulin in last 6 hours (must be stable), x4 (24hr needs) = TDD
- Start with 60-80% of TDD as basal
- Give first dose of basal 2 hrs before stopping drip
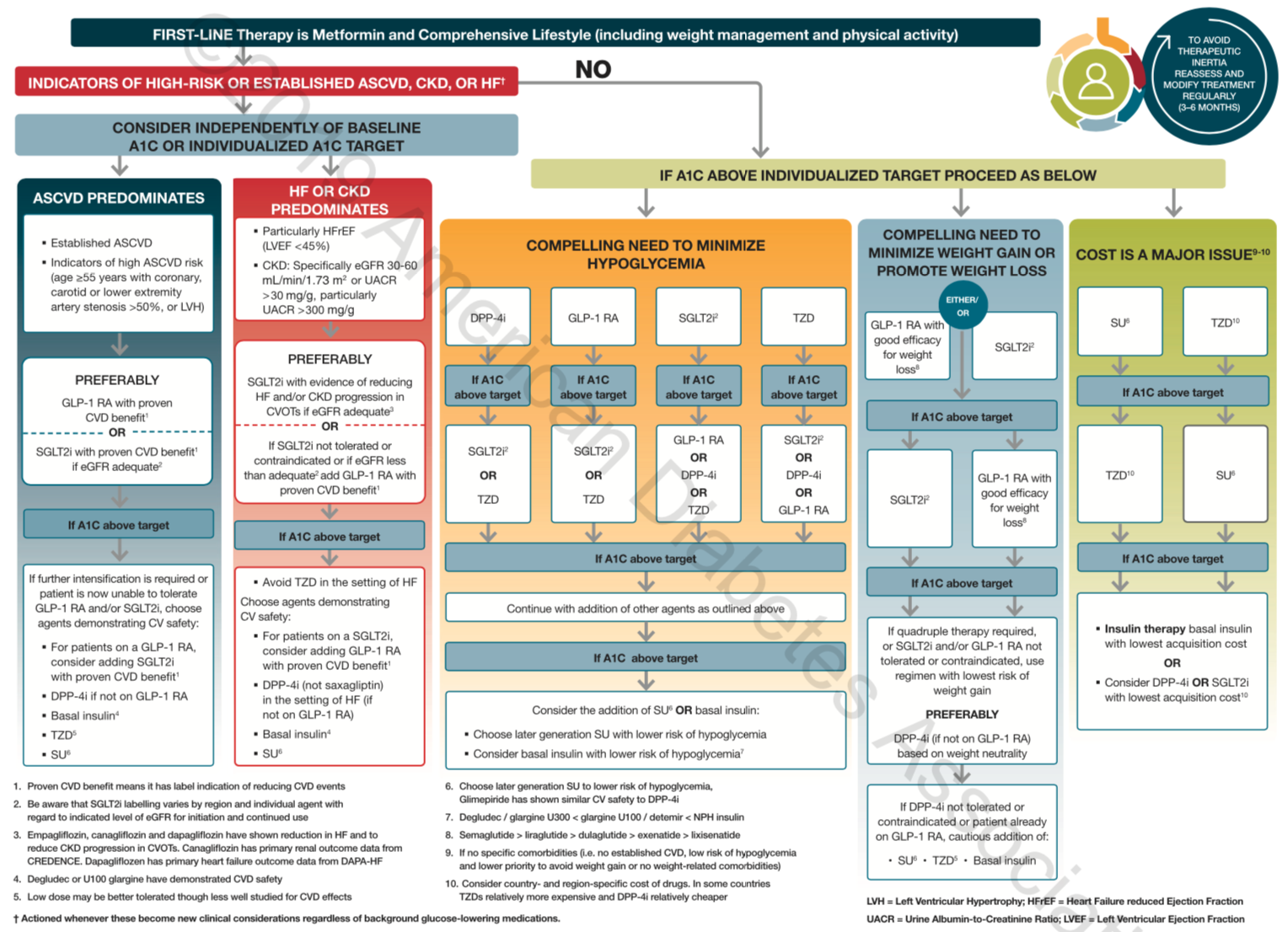
DM2 (Diabetes Type 2) #
A1c >e;6.5% or random glucose >200mg/dL diagnostic.
Outpatient #
Goal: 80-130mg/dL fasting/pre-prandial; <180mg/dL PP with <50mg/dL pre-prandial to post-prandial rise
Treatment #
- Metformin
- Best data on outcomes
- Mechanism: ↓ hepatic production, ↑ insulin sensitivity
- AEs: diarrhea (pt will get this, but will go away), GI upset
- A1c Reduction: >2% (high)
- Ramp on start:
- 500mg qhs x 1 week
- 500mg BID x 1 week
- 1g qAM + 500mg qhs x 1 week
- 1g BID indefinitely
- If not tolerated go to previous step and extend to 2 weeks before up-titration
- Can try ER formulation to minimize GI side effects, still is BID though
- Always take with food (to help with GI upset)
- Long term metformin can cause B12 deficiency, check if neuropathy in any pt on metformin more than 5yrs
- GLP-1 RA, DPP-4, SGLT-2, TZD, vs SU
- GLP-1 RAs ("-tides")
- Mechanism: slows gastric emptying, increased satiety, predictable weight loss (graphic)
- Injections
- daily
- Exenatide (Byetta) (BID)
- liraglutide (Victoza)
- or weekly
- dulaglutide (Trulicity)
- semaglutide
- daily
- AEs: very low risk of hypoglycemia (“smart” secretors), ?pancreatitis, risk of thyroid cancer in pts with strong FMHx (otherwise ok), GI (will get better with use)
- A1c Reduction: >2% (high)
- Sulfonylureas (“g-ides”)
- Glipizide
- “Dumb” insulin secretors (increase secretion regardless of glucose level)
- Think of the using the extended release forms as you would basal insulin
- Always take with meals!
- If you skip a meal, skip a dose
- AEs: hypoglycemia
- A1c Reduction: >2% (high)
- Thiazolidinediones (TZDs)
- Pioglitazone (Actos)
- Increases insulin sensitivity
- potential CV benefits (pioglitazone)
- AEs: edema, caution in HF as edema can mimic HF sx, bladder cancer => caution in pt with strong FMHx (otherwise ok)
- A1c Reduction: >2% (high)
- DPP-4 inhibitors ("-gliptins")
- Linagliptin (Tradjenta)
- Increased insulin secretion (inhibits degradation of GLP-1s)
- AEs: essentially zero risk hypoglycemia, ?thyroid cancer (only seen in mice), ?pancreatitis (never been shown)
- A1c Reduction: 1-2% (intermediate)
- Generally really well tolerated
- SGLT2 inhibotors ("-flozins")
- ertugliflozin (Steglatro), dapagliflozin (Farxiga), canagliflozin (Invokana)
- Mechanism: increased urinary glucose excretion
- AEs: moderate risk of hypoglycemia, UTI, euglycemic DKA (very low risk, but be aware), avoid canagliflozin in pts with foot ulcers
- A1c Reduction: 1-2% (intermediate)
- Take in morning so active during day
- GLP-1 RAs ("-tides")
- Insulin
- Basal
- Normal starting dose 0.1-0.2U/kg/day
- 0.15U/kg/day good fist bet or just start with 10U
- Normal starting dose 0.1-0.2U/kg/day
- Mealtime
- Looking for PP BG to be <180 and total change from pre-prandial to post to be <50 (this is what normal looks like)
- Don’t treat PPs if high but ΔBG < 50; look for highs earlier in the day to treat (i.e. came into that meal high)
- Start with 4U or 10% of basal dose
- Titrate by 1-2U, twice weekly
- Basal
| Med | Hepatic Production | Insuin Secretion | Insulin Sensitivity | Intertinal Absorption | Other |
|---|---|---|---|---|---|
| Metformin | ↓ | ↑ | |||
| Sulfonylureas | ↑ | ||||
| TZDs | ↑ | ||||
| Acarbose | ↓ | ||||
| GLP-1 RAs | ↓ | ↑ | ↓ gastric emptying, ↑ satiety, ↑ weight loss | ||
| DPP-4 inhibs | ↓ | ↑ | |||
| SGLT-2 inhibs | ↑ urinary excretion |
Follow up/Surveillance #
- A1c 2x/yr (or every 3 months if not well controlled)
- Annually
- Lipids
- Creatine
- Foot exam
- Retinal exam
Inpatient #
- Goal: 140-180mg/dL
- Can be higher in older/terminally ill
- Can target lower (<140mg/dL) in right patient if needed
- Do not use just SSI (poor form), need basal too unless needs are decently low
Treatment #
- Orals
- Stop all orals, control with only insulin.
- Resume 1-2 days prior to d/c
- Insulin
- Total needs usually 0.3-0.5U/kg/day
- Usually split about 50-50 between basal and short acting
- Basal
- 0.15U/kg/day (actual weight) is good starting spot
- Uptitrate if fastings are high
- Correctional
- SSI for 24hrs, then can do scheduled or ↑ basal
Common Scenarios #
- Not on insulin
- Hold orals
- If BG <180mg/dL on admit → start just LDSSI
- If needs more than two doses in 24hrs → start basal
- If not, d/c SSI, change to qday BG checks
- If BG >180mg/dL on admit → start basal (0.15U/kg/day) + LDSSI
- Decrease if CrCl <30 (reduced elimination)
- On home basal only
- Continue home dose (can reduce by 20-40% to be safe)
- Add correctional
- On home basal-bolus
- If eating → continue both (can reduce by 20% to be safe)
- If NPO → continue just basal
- On Pre-Mixed
- Add up total daily dose (TDD) of insulin
- if eating → 50% TDD as basal, 50% TDD as scheduled short acting
- if NPO → 50% TDD as basal only
- Add up total daily dose (TDD) of insulin
- On pump
- Verify settings
- Make sure pt has enough supplies while admitted
- Continue pump
- If no, convert to basal/bolus
- Surgery
- Basal/pump: reduce 20-40% for day of surgery
- NPH: reduce 50% morning of
- Orals/mealtime insulin: hold day of
Insulin #
Basal Titration #
- Gut feel => 10-20% changes
- 2x3 Method: ↑2U every 3 days
- Treat to Target (TTT)
- Average fasting BGs over a week, changes every 7 days. If:
- >180: ↑8U
- >160: ↑6U
- >140: ↑4U
- >120: ↑2U
- 303 method: every 3 days if
- >130 (110 if aggressive) increase by 3U
- <80 (70 if aggressive) decrease by 3U
Steroid Induced Hyperglycemia #
Tends to have bigger effect on postprandial glucose.
- If fasting BG > 180mg/dL → consider basal 0.15U/kg/day
- If fasting BG < 180mg/dL and postprandials → consider 0.1U/kg NPH qAM (only)
- NPH has more of a “peak effect”, can target for during day when eating
Thyroid Storm/Severe Thyrotoxicosis #
- Grey line inbetween the two
Treatment #
- PTU 200mg q4h (if thyroid storm) or Methimazole 20mg q4-6h (if severe)
- Propranolol 60-80mg q4-6h
- Hydocortisone 100mg q8h
- Iodine
- Follow fT4
Pearls #
- Correction factor = Change in BG / insulin dosed
- Gives you an idea of how much to use
- Lower numbers → more insulin resistant
- DM2’s usually around 20-30
- DM1’s usually closer to 50
- Gives you an idea of how much to use
- Carb factor = correction factor / 3
- Can pre-dose or know how much to give after meal
- Maximize basal before postprandials
- If BG high, add half of daily SSI dose to basal
- Be sure to order pen needles if rx’ing an insulin pen
- Normal post-prandial glucose rise should be <50 and absolute number should be <180mg/dL