Gastrointestinal (GI) #
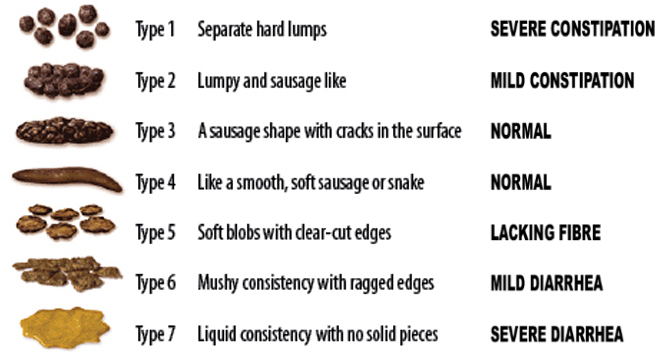
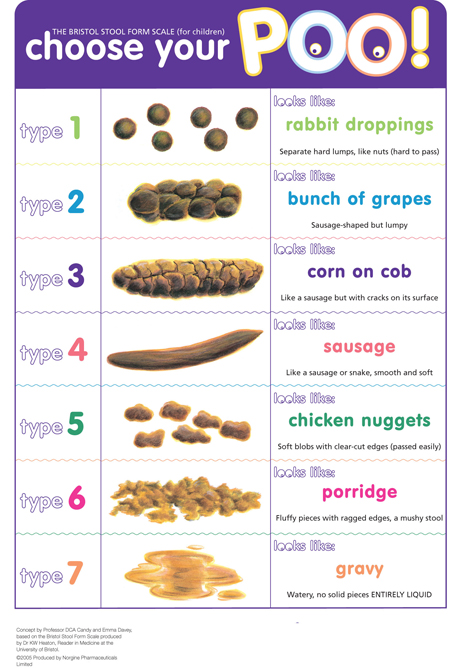
Stool Scales #
Constipation #
- Mirilax + Senna plus
- Bisdocyl suppository
- Soap-suds enema
- Mag citrate (aka “The Nuclear Option”)
Diarrhea #
- loperamide 4mg, then 2mg q2h
- loperamide-simethicone (2mg-125mg)
- Some evidence it works faster than loperamide alone
- octreotide
Nausea/Vomiting #
- Zofran 4-8mg
- inhibits serotonin at 5-HT3 receptors in small bowel, vagus nerve, and chemoreceptor trigger zone
- Qt prolonger
- Compazine (Prochlorperazine) 5-10mg q6-8hrs
- extrapyramidal side effects: restlessness, agitation, akathisia, dystonia, dyskinesia
- Not really a Qt prolonger
- Reglan (metoclopramide) 10mg IV
- Antidopaminergic
- Not really a Qt prolonger
- Zyprexa-ODT 5mg, then 2.5mg q6h prn
- Great for refractory nausea as basically hits all the nausea receptors
- Ativan
- Safe in long Qt
- Benadryl 50mg IV
- Safe in long Qt
- Steroids
- Safe in long Qt
- Haldol?
Abdominal Pain (IBS) #
- Dicyclomine 20mg QID prn
Spontaneous Bacterial Peritonitis (SBP) #
Intrabdominal infection w/o real source
Happens frequently in ESLD patients due to impaired opsonization of bacteria from failing liver
- Paracentesis to dx
- Cell counts and diff
- Cultures (anaerobid and aerobic)
- glucose, total protein, albumin, LDH, amylase
- >250PMNs[^1] in para fluid = SBP
- Correction for hemorrhagic ascites (> 10,000 RBC/mm3) subtract 1 PMN per 250 red
- SBP due to gram-positive cocci frequently reported to have PMN < 250 cell/mm3
- Bugs (most common)
- E. Coli, Klebsiella, pneumococci, Strep viridans, Staph aureus
- Procal can be helpful (small study)
- cutoff of < 0.61 ng/mL
- sensitivity 100%, specificity 92% for SBP
- cutoff of < 0.61 ng/mL
Treatment #
- IV ceftriaxone 1g IV q12h
- Albumin (1.5g/kg IV/6hrs immediately and 1g/kg IV/6hrs on day 3)
- Consider in pts with SCr >1, BUN >20 or total bili >4mg/dL
- Consider stopping non-selective BBs
- Start on norfloxacin 400mg/day PO indefinitely for secondary prophylaxis
Secondary Bacterial Peritonitis (the other SBP) #
Intrabdominal infection w/ real source. Think about this if you think it’s SBP but doesn’t really shake out to be.
- Paracentesis
- <250 PMNs
- Glucose <50mg/dL
- Protein >1g/dL
- Above values limited in sensitivity (<68%)
- Sources
- Gastric perf somewhere
- PUD, Diverticuli, Gallbladder, Appendix, Meckels, post-op anastomosis leak
- Bowel inflammation (generally transmural)
- IBD, Appy, Ischemic bowel
- Gastric perf somewhere
Ascites #
Accumulation of intraparateneal fluid.
Causes:
- cirrhosis (#1, ≈60% incidence in pts with cirrhosis)
- malignancy, nephrotic syndrome, heart failure, malnutrition, and infections (peritoneal TB, coccidioidomycosis, chlamydia), Budd-Chiari
SAAG helps differentiate:
- SAAG ≥ 1.1 g/dL → portal hypertension (cirrhosis) (+LR 4.6)
- Protein < 1 g/dL: Chronic liver disease, massive hepatic mets
- Protein > 2 g/dL: cardiac disease, Budd-Chiari syndrome, veno-occlusive disease, myxedema
- SAAG < 1.1 g/dL → other: peritoneal carcinomatosis, chronic peritoneal infection, nephrotic syndrome, pancreatic ascites, and protein-losing enteropathy
Treatment #
- Antiboitics
- Ceftriaxone
- NNT &qpprox;5
- Ceftriaxone
- Sodium/water restrict
- Avoid NSAIDS
- Decreases renal sodium excretion
- Hold home ACE/ARB, A1-blockers
- Avoid NSAIDS
- Diurese
- spironolactone 100 mg/day (max 400 mg/day)
- furosemide 40 mg/day (max 160 mg/day)
- Therapeutic para
- Can shorten hospital stay
- First choice for tense ascites
- Albumin
- May not effect mortality
- reduces after para hypona,
- Surgery
- TIPS
- Transplant
- Peritoneovenous shunting (Denver shunt)
Cirrhosis #
Fibrosis and regenerative nodules w/ liver dysfunction.
Causes:
- EtOH (most common)
- NAFLD
- Viral hepatitis
- HCV most common in US
- HBV most common worldwide
Diagnosis #
- Workup:
- hepatitis B and C serology
- AST:ALT ratio
- alpha-1 antitrypsin levels with phenotyping
- antinuclear antibody, antismooth muscle titer, antimitochondrial antibodies
- serum ferritin and transferrin saturation levels
- hemochromatosis gene (HFE) testing (if iron saturation is greater than 45%)
- serum copper and ceruloplasmin, and 24-hour urine copper (Wilson’s)
- Lok index (>90% sensitive)
- LogOddsLok = (1.26 * AST / ALT) + (5.27 * INR) - (0.0089 * Platelets) - 5.56
- LokIndex = e(LogOddsLok) / (1 + e(LogOddsLok))
- <0.2: Cirrhosis less likely
- 0.2-0.5: Indeterminate
- >0.5: Cirrhosis likely
- Bonacini cirrhosis discriminant score (>90% specific)
- CDS = PlateletScore + ALTASTRatioScore + INRScore
- <7 => cirrhosis less likely
- ≥8 => cirrhosis more likely
- US
- CT Abdomen
Treatment #
- Transplant ultimately…
- Vaccinate for HepA, HepB and Pneumo23
- Stop drinking!
Acute Pancreatitis #
Diagnosis (2 of):
- Epigastric pain
- Elevated lipase
- Urinary trypsinogen-2 (very specific)
- Imflammation on imaging
Causes:
- Gallstones (≈40%)
- LFTs normal in 15-20% of patients
- EtOH (35%)
- meds (2%)
- analgesics and anti-inflammatory agents
- angiotensin-converting enzyme (ACE) inhibitors
- antivirals (HIV)
- atypical antipsychotics
- corticosteroids
- diuretics
- hypoglycemic agents (antidiabetics)
- macrolides and other antibiotics
- oral contraceptive or hormone replacement therapy, especially estrogens
- proton pump inhibitors
- statins
- thiopurines, including azathioprine and 6-mercaptopurine
- Valproic acid
- hypertryglycerides (1-4%)
- >1000
- trauma (1.5%)
- Most common in kids
- Post ERCP (5-10% of ERCPs)
- Idiopathic (≈10%)
Heartburn #
- No data to support BID PPI as better than Qday
- Theoretical “max” acid supression
- PPI in AM
- H2RA in PM (overnight acid production more histamine driven)
Peds #
Giadariasis #
- Classic Triad: Nausea, diarrhea, stomoch pains/cramps
- Episodic
- Smelly farts
- 20-25 day incubation period
- Usually presents in the fall and paitent have usually dealt with it for a few months
- Tx
- Nitazoxamide 500mg BID pc x3 days
Radiology #
Abdominal CT #
How to read:
- In lung window, scroll down through abdomen looking for free air
- Switch to bone window, scroll back up looking for any bony abnormalities
- Switch to soft tissue window, start with liver/gallbladder, follow ducts down to pancreas
- From pancreas, follow splenic artery/vein to spleen (through pancreas)
- Next find adrenals, kidneys, follow ureters down to bladder
- Trace colon up from rectum
Pearls #
- If pt with C. Diff treated with antidiarrheals, can cause mega colon.
- GGT not specific for hepatobiliary disease (elevated with meds: barbituates, phenytoin, EtOH)
- MELD score to predict mortality in patients with cirhosis.
- homemade recipe for rehydration
- 1 L clean water
- ouncese-half teaspoon salt (3.5 g)
- one-half teaspoon baking soda (2.5 g NaHCO3)
- 8 teaspoons sugar (40 g)
- 8 ounces orange juice (1.5 g KCl)
[^1] PMNs = Neutrophils, Eos, basophils, masts