Cardiac #
AMI #
- Family history is an independent risk factor especially for early AMI. 2.87 RR for early (<55) AMI in women with family history. FMHx is synergistic with other risk factors (high LDL, smoking, etc.).
- Ask about “discomfort” not “pain,” patients tend to be stoic.
- Post-op day 3 → highest thrombotic risk
- NO morphine or nitrates if RV involved => can tank pressures
- T-waves and ↑ for 36hrs, then ↓ for up to 3 weeks
Be sure to be aware of (and document) “anginal equivalent.” (i.e. SOB in old lady with no cp in AMI; sudden onset fatigue.)
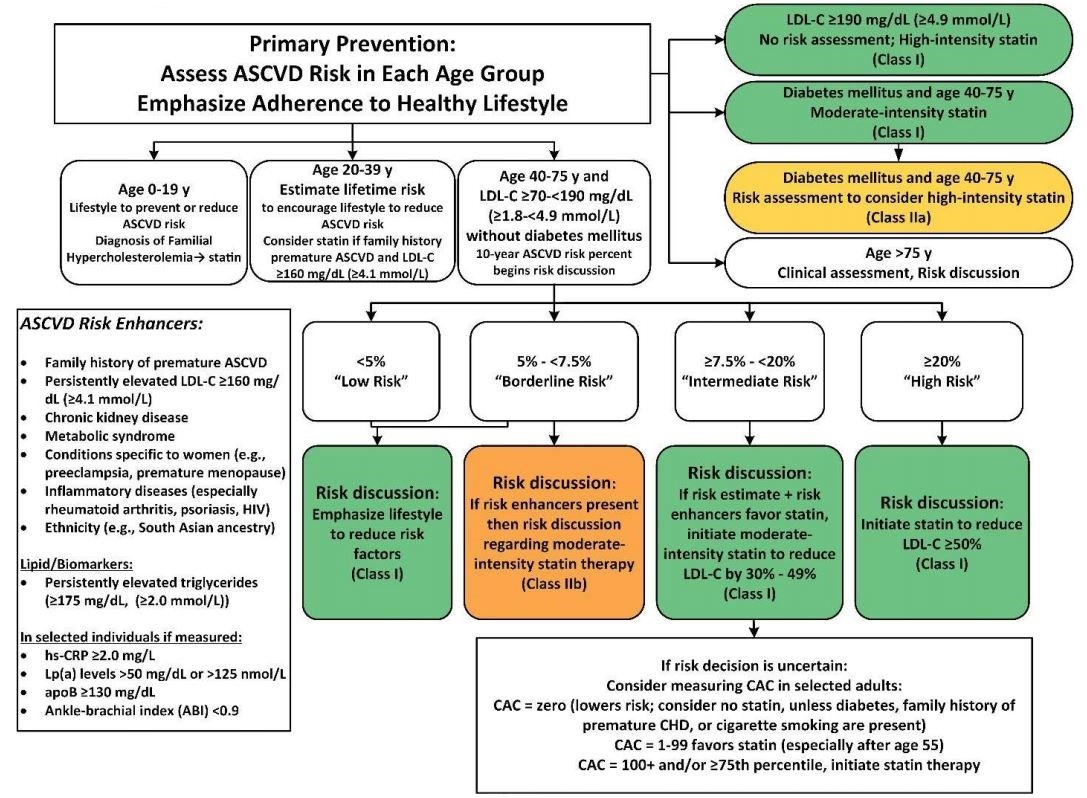
Primary prevention #
AAC Tool with treatment recommendations.
AAC Primary Prevention Algorithm
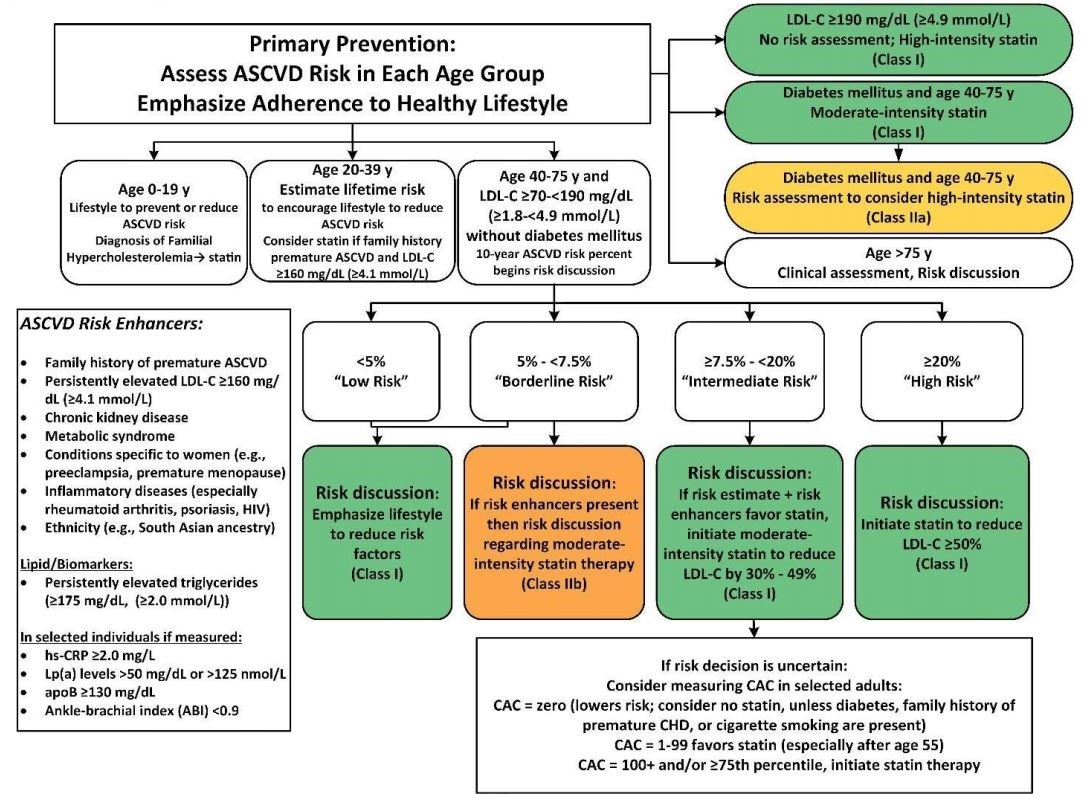
- Age:
- 0-19yo
- Diet/exercise
- ? Familial hypercholesterolenemia
- Diet/exercise
- 20-39yo
- Diet/exercise
- Consider statin if famhx of early ASVCD and LDL-C ≥ 160mg/dL
- High-intensity statin if LDL-C ≥ 190mg/dL
- 40-75yo
- Diet/exercise
- if diabetic
- at least moderate intensity statin
- ASCVD risk
- <5% (low risk)
- Diet/exercise
- 5-<7.5% (borderline risk)
- Diet/exercise
- Moderate intensity statin
- 7.5-<20% (intermediate risk)
- Moderatie intensity statin
- CAC measurement
- zero => consider no statin
- 0-99 => favor statin
- 100+ => initiate statin
- ≥20% (high risk)
- Statin to reduce LDL-C by >50%
- <5% (low risk)
- >75yo
- Clinical judgement/shared decision making
- 0-19yo
Statin Intensity #
| Statin | High Intensity (mg) | Moderate Intensity (mg) |
|---|---|---|
| Atorvastatin | 40-80 | 10-20 |
| Rosuvastatin | 20 (40) | (5) 10 |
| Simvastatin | - | 20-40 |
| Pravastatin | - | 40 (80) |
| Lovastatin | - | 40 |
| Fluvastatin | - | 40 |
| Pitavastatin | - | 2-4 |
- High intensity should lower LDL ≥50%
- Moderate intensity should lower LDL 30-50%
- Doses in (parenthesis) FDA approved but not studied
Comparison of different organization guidelines for primary and secondary prevention.
Pre-op Clearance #
Based on 2007 ACC/AHA Guidelines.
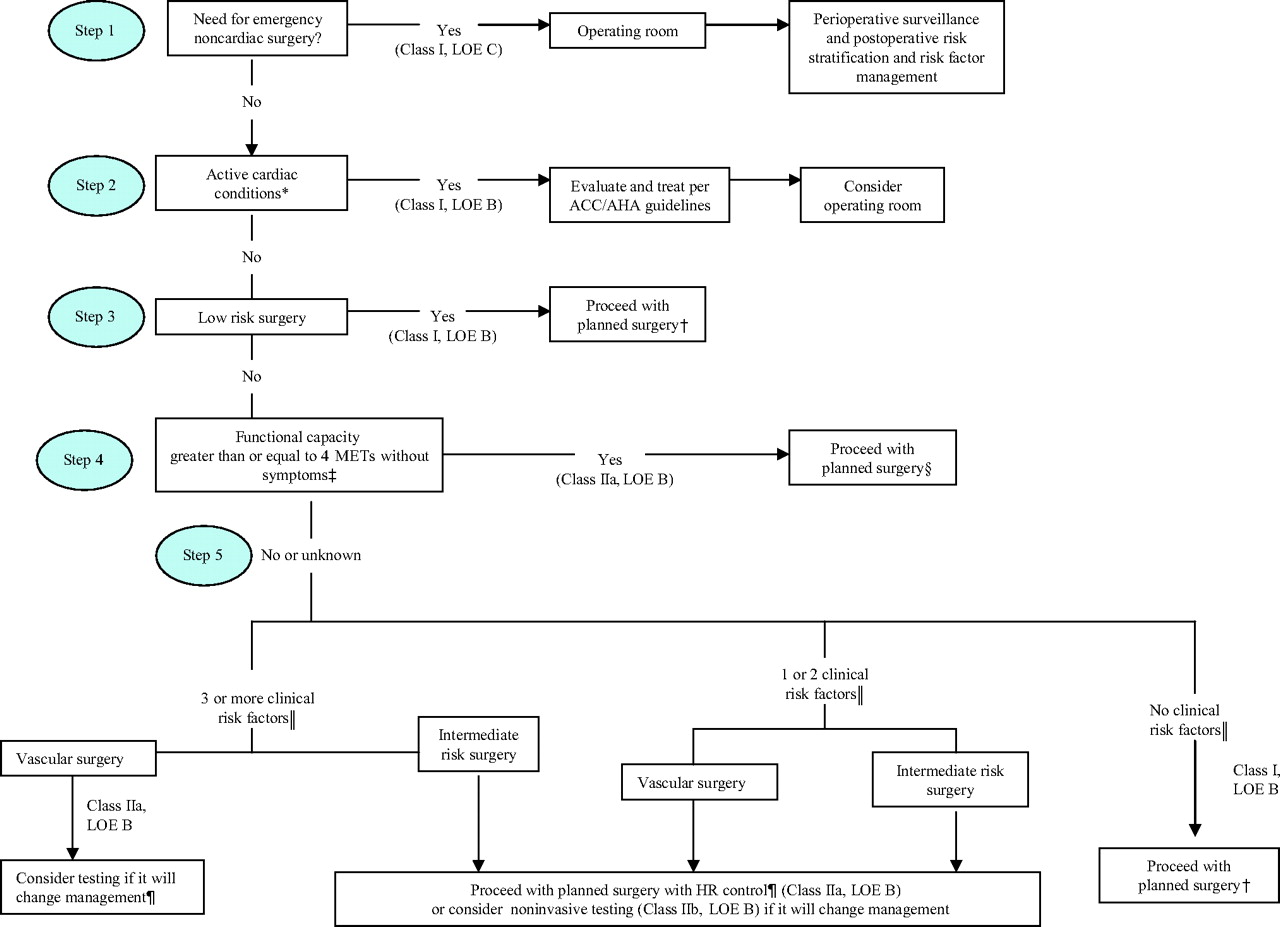
Surgery Risk #
| Low (<1%) | Intermediate (1-5%) | High (>5%) |
|---|---|---|
| Endoscopic | Abdominal | Aortic |
| Superficial/skin | Thoracic (non-cardiac) | Peripheral vascular |
| Eye | Head/Neck | |
| Breast | Orthopedic | |
| Ambulatory | Prostate | |
| Carotid Endartectomy |
- 4 METS = going up flight of stairs
- HTN not coorleated with adverse outcomes, but should probably treat SBPs >180 before surgery
CHF Management #
Neumonic: Paris
-
Preload => loops, symptomatic only (no mortality benefit)
-
Afterload => ACEI/ARB
-
Remodeling => ACEI/ARB, BB, Spirolactone (mortality benefit)
-
Ionotrope/Iron => Milronone, Dobutamine, Digoxin (↓ hospitalizations), Iron
-
Shock => ICD, EF <30%
-
CCB’s in HF reduce EF in the long term
HFrEF (EF<40%) #
- ACE (probably ARB), BB => mortality benefit
- Diurese
- Consider imdur/isordil + hydral if need more BP control
- If kidneys ok => switch ACE for spironolactone
HFpEF (EF >40%) #
- No therapies with proven mortality benefit (unlike HFrEF)
- Control BP with BB, ACE/ARB
- Consider pulm artery pressure monitoring
Tool to estimate benefit of meds.
Diuretic Conversions #
| Form | Lasix | Bumex | Torsemide | Ethacrynic acid |
|---|---|---|---|---|
| IV | 20mg | 1mg | NA | ??? |
| PO | 40mg | 1mg | 20mg | 50mg |
-
Lasix 1:2 IV:PO
-
Bumex 1:40 Lasix
-
Bumex 1:1 IV:PO
-
Bumex possibly the worst loop (shortest duration with rebound Na retention)
-
Torsemide best loop on paper with longest duration of action although no IV option
EKG #
Practice 12-Leads
Dr. Nelson’s EKG Book
Big Box = 200 msec
Little box = 20 msec
Reading Approach #
- 10,000ft view: Regular? Irregular? Grouped beating? Glaring abnormalities?
- Sinus? P-waves upright in I and aVF
- Not same number of P’s and QRS’s? -> Figure out rhythm
- Axis: Lead I and aVF
- If LAD: IMI vs LAFB (vs LVH => rare, need a ton of extra muscle to really deviate it)
- If RAD:
- Rate
- 300-150-100-75-60 rule
- total complexes in rhythm strip x 6
- 60 ÷ msec R-R duration
- Intervals: PR, QRS, QT
- QT trick: not prolonged if less than half of R-R duration
- QTc = QT/sqrt(R-R)
- QRS: Narrow, wide or wide-wide?
- Look at I, aVL and V6 for bundles
- RBBB
- S slurred, slow repolarization
- LBBB
- R slurred upstroke with abnormal repolarization
- RBBB
- Look at I, aVL and V6 for bundles
- If grouped beating: constant PR interval?
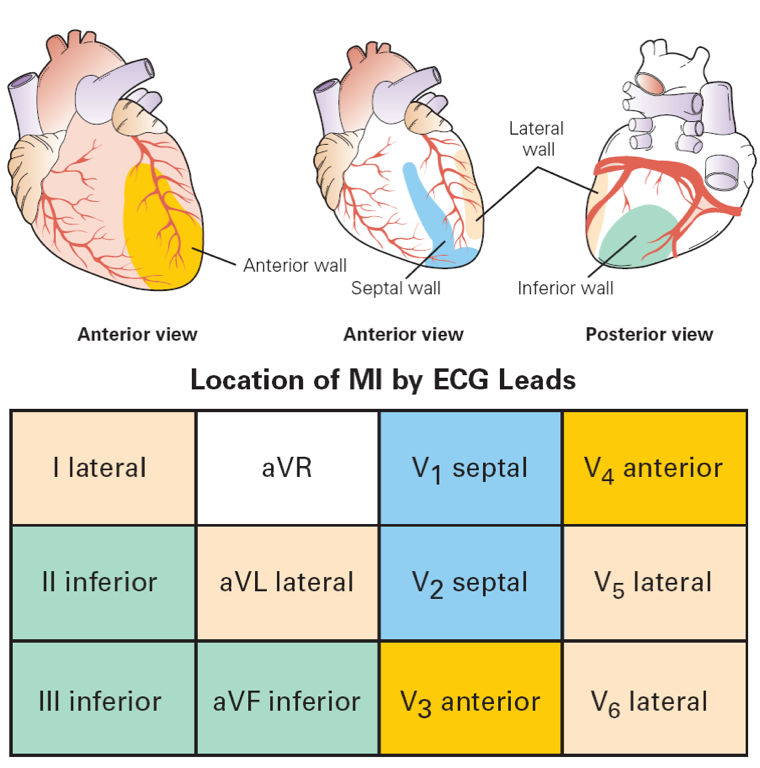
- “Dead stuff:” find pathologic Q waves (>25% of R)
- ST segment abnormalities: Look for recipricol changes whenever possible
- Inverted T’s can help with time course of MI
EKG Pearls #
- Lead I completely flat (Shamroth’s Sign)
- hyperinflation lung disease (COPD), heart essentially with a North-South axis
- RBBB
- R+R’ in V1-2
- V6 with deep S and slow repolarization (most sensitive)
- also seen in I, aVL
- inverted T’s in V1-3
- Can still interpret everything normally, really only see the LV on EKG anyway
- Avg QRS width ≈120msec
- LBBB
- Wide QRS in I and mostly down in V1
- can have a small “septal” Q in V1 which is actually RV free wall
- Avg QRS width ≈140msec
- Cannot interpret rest of EKG, except:
- concordant ST elevation
- ST depression in V1-3 (should be elevated) => posterior MI
- Discordant ST elevation of more than one big box (>5mm)
- Q-waves in I, aVL or V6 => anterior septal infarct of indeterminate age
- LAFB (thnk anterior superior)
- no clinical importance
- LPFB (think posterior inferior)
- very burley fascicle, very hard to mess up by itself
- dx of exclusion
- RBBB + LAFB => only posterior fascicle is working
- not good if intermittent, only one fascicle that’s actually working and it’s intermittent…
- DDx: giant negative T waves
- pericarditis
- pheo
- takotsubo’s
- myocarditis
- DDx: Left axis deviation
- Massive inferion MI
- LAFB
- LVH (rarely)
- T-waves in AMI are ↑ for 36hrs, then ↓ for up to 3 weeks
- If have Q waves in I, aVL, or V6 with LBBB => anterior septal infarct of intederminate age
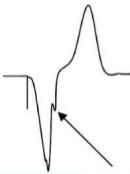
- Cabrera’s sign => AMI in LBBB, look in V3-4 for notch in ascending S wave
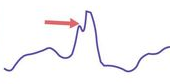
- Chapman’s sign => AMi in LBBB, look in I, aVL, V6 for notch in ascending R wave
- DDx for poor R wave progression: Anterior MI, LVH, LBBB, Severe COPD; things that push the heart: L pneumothorax, effusion, amyloidosis/hemochromatosis, tumor inflitrates.
- Last part of the QRS in V1 tells the bundle: ↑ right bundle, ↓ left bundle.
- RVH criteria
- Right axis deviation (9 times out of 10 is RVH)
- R>S in V1 or R >7mm
- LVH criteria (need 5 points to call LVH, 4 is probable)
- Left atrial abnormality (3pts)
- notched P’s in V1 if neg portion of P in V1 more than one little box
- R or S in limb leads >20mm OR (3pts)
- S in V1-3 >25mm OR
- R in V4-6 >25mm
- ST segment shift (any, no digoxin) (3pts)
- Left axis deciation of >-150 (2pts)
- Left atrial abnormality (3pts)
- LV “strain” pattern
- ST depressions, Large T + inverted T in V5-6 (sometimes I, aVL)
- RV “strain” pattern
- ST depressions, T-wave abnormalities in right heart leads: V1-3(4), II, III, aVF
- Flutter
- 1 big box ± 1 small box
- Big Q’s + ST elevation = LV anyurism
- WPW with syncope => cath immediately
- without syncope can do outpatient EP study
- Cannot interpret anything on WPW beats as isn’t going through the right pathway
- Early repolarization doesn’t happen to females
- Adenosine “poisons” the AV node temporarily
- “Hyper” things (↑K, ↑Ca) shorten Qt
- “Hypo” things (↓K, ↓Ca) lengthen Qt
- Most common cause of polymorphic VT is MI
Blocks #
AV #
- AV node and higher responds to atropine
- Use pacemaker if symptomatic
- Below AV node requires pacemaker
- If in AV node
- Type I winkeback or long PR
- Can use meds to treat
- good “real estate” as works sometimes
SA #
- Grouped beating with missing P-waves
- SA node just can’t depolarize the atria for some odd reason
QTc #
Normal QTc:
- Men: 440
- Women: 460
In general, don’t worry about Qtc < 500
QTc >500, worry about increased risk for torsades
Qtc = Qt / sqrt(R-R interval)
Qt prolonging meds hit the fast K channels
K > 4.0, Mg > 2.0 reduces risk of torsades with prolonged QTc
List of QT prolonging drugs
Leads #
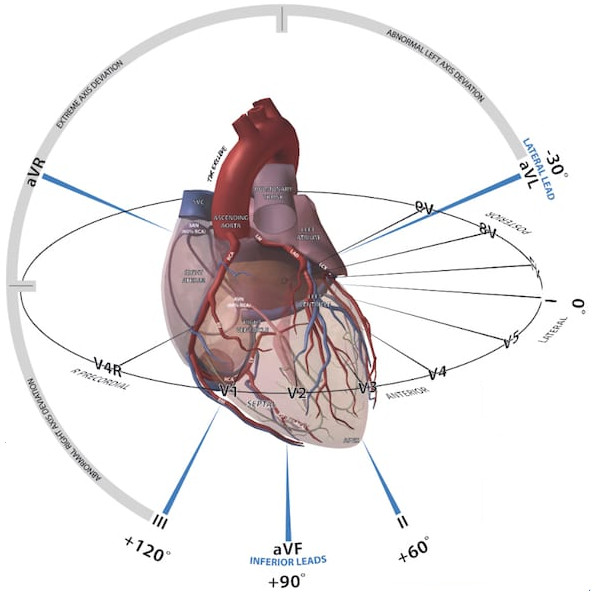
LII LI ASS up ALL down
Tachycardia #
First question: narrow vs wide?
Narrow QRS #
- no visible p-waves? => indicates atrioventricular nodal reentrant tachycardia (AVnRT) or atrioventricular reciprocating tachycardia (AVRT)
- if has p-waves
- More p’s than QRS
- A-Flutter
- atrial tachycardia
- 1:1 p’s to QRS’s
- Short PR
- < 90 ms => AVNRT
- > 90 ms => AVRT, atypical AVNRT, or atrial tachycardia
- Long PR
- atrial tachycardia
- sinus tachycardia
- atypical AVNRT or AVRT (rare)
- Short PR
- More p’s than QRS
Pericarditis/Pericardial Effusion #
Worry about tamponade. DO NOT give lasix, even if volume up, as they’re preload dependent, risk heart failure.
CXR can be normal, need >200mL of effusion before cardiac sillohete enlarges.
Causes:
- Idiopathic/Viral (80-85%)
- Malignancy (5%)
- Autoimmune (5%)
- TB (in the right setting)
EKG Changes #
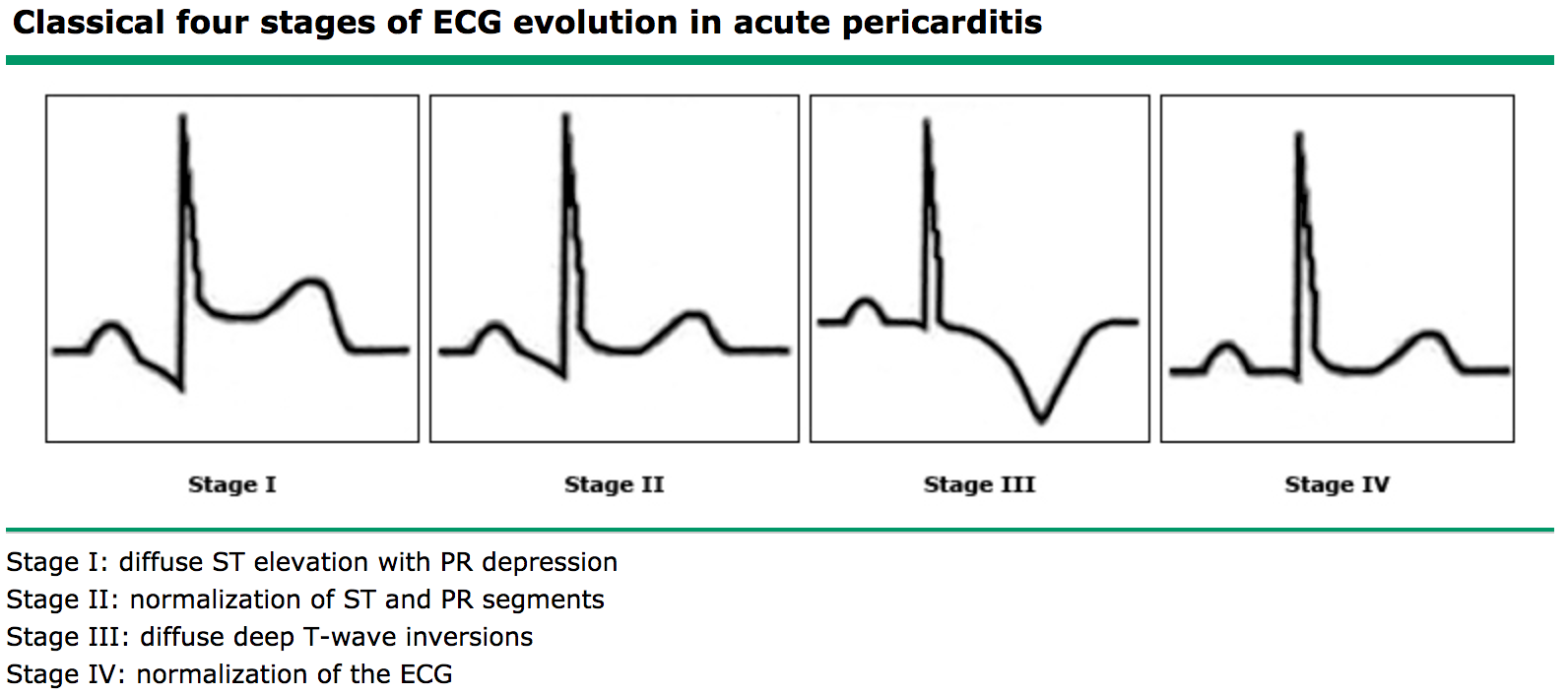
Treatment #
NSAIDs + colchicine
- Ibuprofen 600-800mg TID (Add PPI if worry about gastritis)
- Colchicine 0.6mg Qday (BID if >=70kg)
Can use glucocorticoids if needed.
Atrial Fibrillation (Afib) #
- Intermittent afib is ok!
- Do not necessarily need to be admitted to tele, pulse ox monitor ok for rate.
- Most spontaneouly convert out of afib in ≈5 days
- Uncommon under 60 (≈5% of population)
- >60yo ≈20% of population
- >80yo ≈30% of population
Rate control before rhythm control.
Rate Control #
Acute #
- Metoprolol 5mg IV, q2 minutes x 3
- Diltiazem 0.25mg/kg bolus, then IV infusion
- Amiodarone 300 mg IV over 1 hour, then 10-50 mg/hour IV over 24 hours
Chronic #
Use beta blockers. Shoot for <110. No difference in outcome between HR <80 and <110. Be more worried about bottoming HR out.
- Metoprolol (CAD)
- Carvedilol (CHF)
Metoprolol give less decrease in BP than carvedilol.
Digoxin only if patient is hypotensive.
Rhythm Control #
Amlodapine => great short term, bad long term
Good option for old patients with normal lungs
Flecainamide (Class Ic antiarrythmics)
Good option for young patients with normal heart. Must be used with BB as it “greases” the AV node.
Dronedarone => Good for patients with lung disease. Safer, but less effective and more expensive.
Anticoagulation #
SparcTool for aticoag calculations and options.
Wafarin #
Vitamin K antagonist. Inhibits synthesis of factors II, VII, IX and X (and Protein C & S).
| Factor | Halflife (hrs) |
|---|---|
| II | 42-72 |
| VII | 406 |
| IX | 21 |
| X | 27-48 |
| Protein C | 6-9 |
| Protein S | 5-60 |
- Load with 10mg x 2 days, then titrate to INR
Warfarin target INR 1.7-3.0.???
Tons of interactions. Most notable: - ↑ INR - Metronidazole - Bactrim - -azole antifungals - ↓ INR - Nafcillin - Rifampin - carbamazepine - phenytoin - cholestyramine
DOACs (Direct Oral Anticoagulants) #
| Med | Mechanism | Dosing | Reversal | non-valve afib | PE/DVT tx | PE/DVT Prophylaxis | Surgery | Notes |
|---|---|---|---|---|---|---|---|---|
| Rivaroxaban (Xarelto) | Xa inhibitor | BID - qDay | andexant alfa | Yes | Yes | Yes | Yes | +CAD/PAD tx w/ ASA |
| Dabigatran (Pradaxa) | Direct thrombin inhibitor | BID | Idoracuzmab (Praxbind) | Yes | Yes1 | Yes | Hip | |
| Apixaban (Elliquis) | Xa inhibitor | BID | andexant alfa | Yes | Yes | Yes | Knee, hip | |
| Edoxaban | Xa inhibitor | Daily | None (andexant alfa should work) | Yes | Yes | Yes2 | Cannot use in normal kidneys | |
| Betrixaban (Beryxxa) | Xa inhibitor | Daily | None (andexant alfa should work) | Yes3 |
DOACs ("-xabans") are safer than warfarin; less bleed risk. Easy to hold before procedures:
- Minor procedure: hold 1 day before
- Major procedure: hold 2 days before
CPR #
In hospital, survival to d/c => 18%, about 50% of those patients do well long term.
Patients that do best:
- Young
- Heart failure (Vfib/tach => shock)
- Surgical patients
Patients that do poorly:
- Old/Nursing home patients
- Cr >1.5
- Metastatic Cancer
- COPD
- Sepsis
ASCVD Risk and Primary Prevention #
Physiology #
Intrinsic rate of heart cells:
| Cell | Rate | Notes |
|---|---|---|
| Sinus Node1 | 50-100bpm | can get in to the 30-50 range overnight |
| AV node1 | 45-60bpm | |
| Ventricular conduction cells | 30-45bpm | |
| Ventricular myocyte | 20-30bpm | |
| Atrial myocyte | <20bpm |
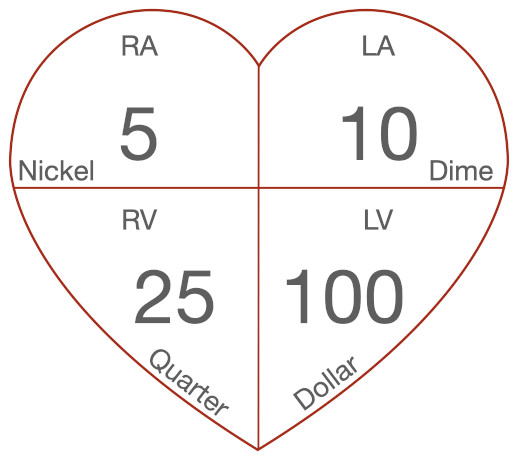
Normal Pressures:
Pearls #
- Kardia: Long term event monitor useful for rare/minimal monitoring
- Loud P2 => usually pHTN
- Tachy-brady syndrome: afib at 140s, with treatment HR drops to 40s; dammed if you do, dammed if you don’t
- PADUA score for determining need for SCDs vs pharmacologic DVT prophylaxis
- Young women can have spontaneous coronary dissection
- Midodrine: global vasoconstrictor (think of it as oral levophed, or levophed “lite”)
- Octreotide: specific splanchnic vasoconstrictor
- Holter monitor is “world’s most useless test”
- Can’t make asymptomatic people better
- Event monitor more useful
- Worry about asyncopal cardiac pauses >3.5 seconds at night
- Wide pulse pressure (High/normal SBP, low DBP) Ddx: Aortic valve disease, stiff vessels (athlerosclerosis)
- Biggest cause of otherostatic hypotension => antihypertensives
- Ask about recent changes to meds
- Digoxin
- Increases automaticity => faster SA rate
- Increases vagal tone => longer PR
- All other drugs make SA faster and PR shorter
- Be suspicious of digoxin toxicity with high rates and dropped beats
- “Rich emotional experience”